Osteopathic Revolution in Veteran Health Care
Osteopathy Offers Veterans a Path to Physical and Emotional Wellness at Mare Island VA Clinic and Gives Student Doctors an Opportunity to Help

For the Chief Medical Officer of the Mare Island and Fairfield VA Clinics, Dr. Dru Herring, the dream is to create a formalized osteopathic program within the Veterans Affairs Clinics.
“I commonly work with patients who have a history of traumatic brain injury, musculoskeletal trauma, various stages of recovery from surgery, and military service-connected disabilities,” says Herring. “In my experience, osteopathy has been able to support veterans with complex disorders, such as PTSD, postoperative spinal and brain surgery, Guillan Barre, Polymyalgia rheumatica, Ehlers Danlos, and Myasthenia Gravis.”
The program is still developing, and to expand the services, Herring began precepting clinical rotations for students in Doctor of Osteopathic Medicine programs. The hope is for a partnership with Touro University California (TUC) that could potentially staff more osteopaths to expand the number of treatments the clinics can offer. In the first-year trial, TUC student doctor Heidi Molga participated in the program.
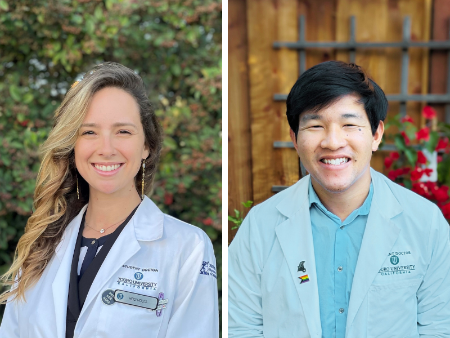 “There is a lot of integration, clinically, with respect to the osteopathic perspective on all of those illnesses,” says Molga, pictured on the left. “We owe it to them to give them the best treatment that's available, which includes providing Osteopathic manipulation in addition to the other medical treatment that they're getting.”
“There is a lot of integration, clinically, with respect to the osteopathic perspective on all of those illnesses,” says Molga, pictured on the left. “We owe it to them to give them the best treatment that's available, which includes providing Osteopathic manipulation in addition to the other medical treatment that they're getting.”
One patient they assisted has been suffering with debilitating back pain. Because of the physical anguish, the patient would end up in the ER, be given a shot of the pain killer Toradol, and sent home. Yet after a few OMT sessions with Herring, the patient saw increased mobility and a decrease in pain and spastic episodes according to Molga.
Most of the VA patients have never heard of osteopathy, says Herring, but once they experience it, they usually recommend it to others. Since Herring got approval to start the OMT clinic a year ago, demand has become so high that Herring has a waiting list. Herring’s OMT program at Mare Island and Fairfield are the first dedicated osteopathic systems at the Northern California Department of Veterans Affairs.
“The osteopathic approach is meeting the patient where they are,” says Herring. “When patients have experienced trauma, the approach is more subtle and gentle, so that you can support them and help their nervous system sustain a state of calm and balance.”
The program is still developing and expanding the availability of OMT services. The hope is that a partnership with TUC could potentially staff more osteopaths to expand the number of treatments the clinics can offer. In the first-year trial, TUC student doctor Heidi Molga participated in the program.
TUC student doctor Anthony Yeh, (pictured on the right) who also did a rotation with Herring, said that OMT also helped patients with post-operative issues.
Yeh says that they saw patients who had surgical procedures like appendectomy, gall bladder removals, or kidney biopsies, which had left some restrictions on their abdomen. Similar issues were found with a patient who had throat cancer. With both types of patients, Yeh says that OMT sessions were able to release restriction with the diaphragm, bringing pain relief and more.
“What we saw at the end of each session was that patients seemed physically lighter, moving in a more fluid motion, and more relaxed,” says Yeh.
The OMT program is something that Herring sees as an important compliment to the array of wrap around services the VA Clinic offers veterans that include psychotherapy, whole health coaching, exercise, recreational therapy, and dietitians in addition to primary care.
“This supports patient wellness and aligns with the goals of osteopathic treatment,” says Herring. “It’s very encouraging as a physician that after your patient leaves, you can also provide them support tools to help them with their self-regulation and wellness.”
Herring hopes to expand the program by offering more rotation opportunities to Touro student doctors that have already made a positive impression on both Herring and the patients. Herring says that the Touro students she’s worked with are grounded, kind, perceptive, and sharp.
“I cannot overstate how impressed I am with the Touro students I have worked with,” says Herring. “Working with students keeps me on my toes and reinvigorates what I love about this profession.”
